Edit Content
The integration of POCUS into HIV/TB protocols provided a more comprehensive approach to patient care, addressing multiple aspects of the diseases in a single diagnostic session.
In the early hours of a quiet night at a rural sub-Saharan hospital, a 36-year-old woman of African descent arrived, accompanied by her husband. It was 2 a.m., and the patient presented with complaints of intense lower pelvic pressure. The hospital was staffed by a midwife, with no obstetrician or radiologist on site. However, the midwife had participated in and was certified through a basic POCUS obstetric ultrasound course sponsored by the hospital.
Upon physical examination, the midwife noted that the patient’s uterus was hard and contractile, which raised concerns about a potential complication in the pregnancy. Recognizing the limitations of her physical examination, the midwife decided to utilize her POCUS training to gather more information.
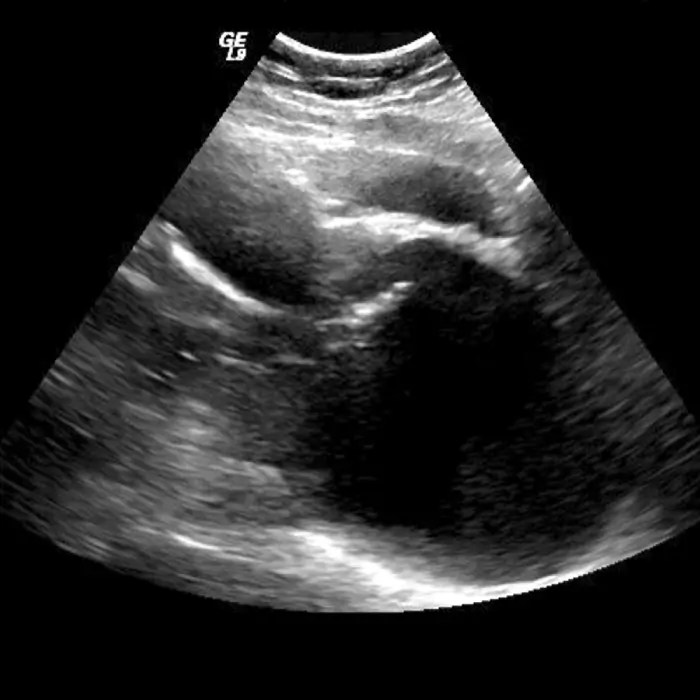
Using the portable ultrasound device, the midwife conducted a thorough ultrasound examination. Initially, the fetus appeared normal with appropriate biometric parameters. However, when examining the maternal lower uterine segment and cervix, the ultrasound images appeared unusual to the midwife.
Confident in her training but cautious about the abnormal findings, the midwife transmitted the ultrasound images to the on-call sonologist using the hospital's tele-imaging system. This enabled expert review and interpretation of the images remotely.
The sonologist reviewed the images and diagnosed cervical incompetence, a condition where the cervix prematurely dilates during pregnancy, leading to a risk of spontaneous abortion or preterm birth. Swift action was taken to perform an emergency cerclage, a procedure where the cervix is sewn closed to maintain the pregnancy.
The procedure was successful, likely preventing a spontaneous abortion and contributing to the continuation of a healthy pregnancy. The timely POCUS diagnosis and intervention highlighted the critical role of ultrasound skills in rural settings where specialist access is limited.
OUR WORK IN
This case underscores the importance of POCUS training for midwives and other healthcare providers working in rural and resource-limited environments. The midwife’s ability to identify abnormal ultrasound findings and utilize tele-imaging for specialist consultation was pivotal in ensuring a positive clinical outcome. This scenario emphasizes the potential of POCUS to enhance diagnostic capabilities and improve maternal-fetal care in settings where traditional radiologic resources are unavailable.
Blogs, case studies, and technical resources around our work in Kenya.
